What I take away from all of this info is that we need to keep an open mind and continue questioning the research.
Dianne Kelecy, MS, RD, LDOncology dietitian Dianne Kelecy, MS, RD, LD, reviews recent studies and recommendations for calcium intake and gives helpful tips to make sure you’re getting enough of this vital mineral.
What is calcium?
We in Oncology Nutrition Services often get asked about vitamins and minerals linked to cancer. One of these is the most abundant mineral in the body: calcium. While 98 percent of that makes up our bones and teeth, it keeps our tissues solid and flexible. It's also involved with muscle function, blood vessel contraction and dilation, blood clotting, nerve transmission and hormone secretion. And calcium does not act alone. It works hand in hand with a long list of other vitamins and minerals in our body.
Where is it found?
Found naturally in some foods, such as dairy, calcium is often added to other foods. It’s also present in some medications, such as antacids, and is widely available as a dietary supplement.
So how much do we need?
Calcium is absorbed less efficiently as we age, which is kind of a bummer, but one of the many reasons we need a little more as we get older.
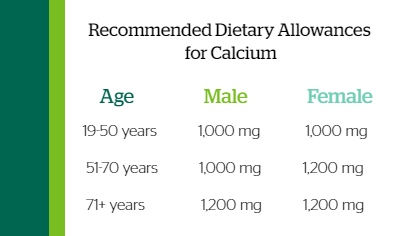 Recommended dietary allowances are 1,000 mg of calcium for men and women ages 19–50 years. From 51–70 years, men stay at 1,000 mg, but women bump up to 1,200 mg. That's mostly due to the hormone shifts of menopause and the increased risk of bone loss that starts to occur at that time. Men and women over age 70 should be targeting 1,200 mg of calcium daily.
Recommended dietary allowances are 1,000 mg of calcium for men and women ages 19–50 years. From 51–70 years, men stay at 1,000 mg, but women bump up to 1,200 mg. That's mostly due to the hormone shifts of menopause and the increased risk of bone loss that starts to occur at that time. Men and women over age 70 should be targeting 1,200 mg of calcium daily.
There is such a thing as too much calcium. The safe upper limit is 2,000 mg daily for those older than 51 and 2,500 mg daily for those ages 19 to 50. In the presentation, we break down the bioavailability of calcium, or amount that is actually absorbed by the body. I also explain how to read nutrition and supplement labels to know how much calcium you’re really getting. Finally, I describe who, based on diet or increased risk of bone loss for several reasons, is most likely to need a calcium supplement.
The “C” connection
What role does calcium play in cancer? Sometimes there are high blood calcium levels when cancer is present. There are two main reasons for this: If cancer has already spread to the bones, it's causing a release of calcium into the blood. The tumor can also create a hormone that interferes with normal calcium levels.
Elevated blood calcium levels are seen in 20–30% of cancer patients, most commonly myeloma. But we also see it most often in breast, lung, kidney and prostate cancers. In the presentation, we’ll go over some symptoms a person with high calcium might feel.
Treatment for certain cancers may also come with a recommendation from your doctor or nurse practitioner to take a calcium supplement. Aromatase inhibitors used to treat estrogen-receptor positive or ‘ER+’ breast cancer accelerates bone loss beyond typical rates seen with menopause. As an oncology nutritionist, I advise ER+ breast cancer patients on an aromatase inhibitor to make sure they’re getting enough calcium—around that 1,200 mg amount—between diet and supplements combined.
Men with prostate cancer may be on androgen deprivation therapy (ADT), which promotes osteoporosis. It's possible that men on ADT might be advised to take a calcium supplement. However, we do hear that calcium promotes prostate cancer and often get asked ‘why would I take more of it?’ That is a very legitimate and difficult question to answer.
Evidence-based information
In my video presentation, I summarize 8 studies as highlights of what’s out there and important points to consider about each. What I take away from all of this info is that we need to keep an open mind and continue questioning the research. When you hear a mainstream broadcast, remember there's probably more to those studies than what they report.
What I can say is that it’s important to meet recommended dietary calcium allowances with food and supplement combined. And as always, continue to eat as many plant foods as you can for so many other benefits.
Kelecy’s full presentation is also available on the Dartmouth Health YouTube channel.